Macular degeneration – Types, causes, and remedies
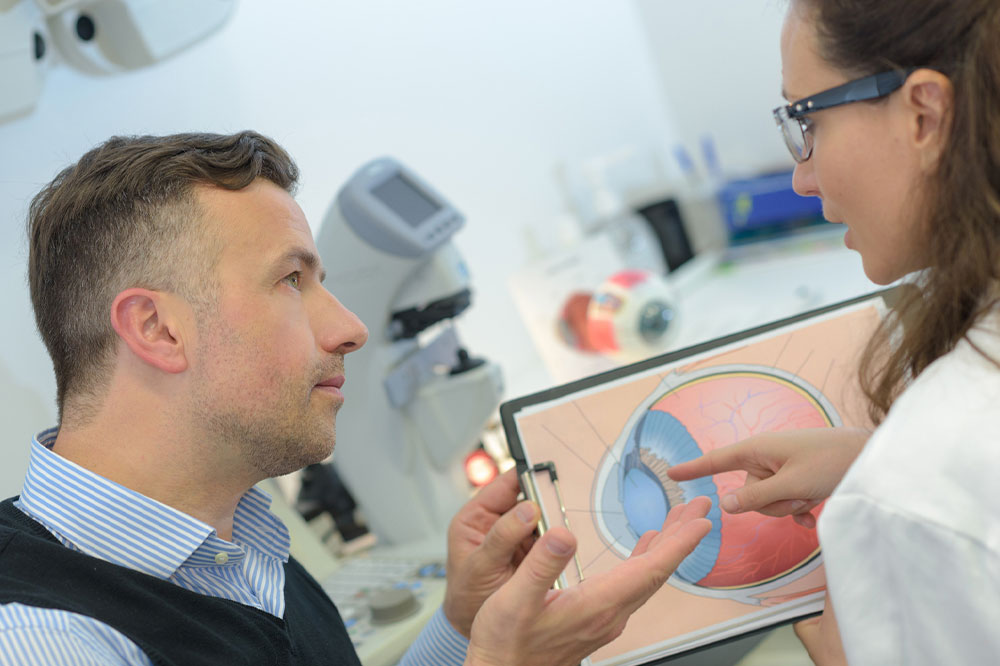
Macular degeneration is a condition that affects a person’s vision and develops as people age. This progressive eye disorder involves the deterioration of the macula, which is a part of the eye’s retina. It is a leading cause of vision loss in older adults and may develop in one or both eyes. This condition is of two main types – dry and wet. Read further to learn about the disorder, its causes, and its types.
Dry macular degeneration
People are more likely to have dry macular degeneration than wet form. It is also less severe and develops when tiny yellow protein deposits under the macula. These deposits dry and thin the macula, causing gradual central vision loss while the peripheral vision remains intact. In the advanced stages, the dry form can progress to the wet form. People with dry macular degeneration need to test their eyes daily at home using an Amsler grid. One must consult a health expert immediately if any vision changes are observed.
Wet macular degeneration
In this condition, the blood vessels grow beneath the retina and macula and cause blood and fluid to leak into the retina. This build-up of fluid results in scarring, leading to permanent loss of central vision. The wet form can cause a sudden change in eyesight resulting in a severe loss of centralized vision when left untreated. People with wet macular degeneration may require repeated treatments.
Symptoms
Macular degeneration may not cause any symptoms during the early stages. However, as the condition progresses, it can cause distortion and blurry vision. It can result in difficulty reading, driving, and identifying colors. Macular degeneration occurs mainly in people aged over 50.
Blurred vision
Dark, blurry areas appear in the center of the vision, leading to increased blurriness in reading printed words.
Visual distortion
The person may experience visual distortions, such as straight lines that look wavy or crooked, and objects may appear distorted.
Need brighter light
It is one of the early symptoms of macular degeneration. Those affected may find reading hard or require brighter light when reading.
Difficulty recognizing faces
People may also have difficulty recognizing faces and facial expressions.
A dark spot in the field of vision
As the condition worsens, people may get a blind or dark spot in the middle of the visual field. This blank spot may also become larger as the disease progresses. Depending on the severity, visual loss can occur within months or years. If you are experiencing any of these symptoms, visit an eye specialist as soon as possible.
Causes
Researchers are yet to find out the exact cause of macular degeneration. However, certain factors may increase your risk of macular degeneration. For example, this eye condition is more common in people over 50. Family genes are linked to this condition. A person’s risk is higher if a close family member has this condition. The risk of macular degeneration increases in people who lead unhealthy lifestyle habits. An unhealthy BMI also increases the chance of developing macular degeneration and the risk of progressing to a more severe form. Consuming saturated fats in foods like butter, cheese, and meat increases the risk. A person is at a higher risk of developing this eye disorder if they suffer from cardiovascular disease.
Stages of Macular Degeneration
Macular degeneration occurs in three stages – early, intermediate, and late/advanced stages. Regarding early-stage macular degeneration, medium-sized deposits form in the retina causing changes in the macula, but vision is not affected. In the intermediate stage, there will be large-sized deposits with mild vision loss. The dry or wet form that causes loss of central vision is an indicator of late or advanced-stage macular degeneration. The time it takes for the condition to progress from early to late stage depends on factors like the size of the deposit.
Remedies
Though there is no cure for macular degeneration, there are a few tips to prevent the condition from worsening.
Include leafy greens in your diet
Leafy greens contain vitamins and antioxidants, including lutein and zeaxanthin, that help protect against cellular damage. To slow down the progress of macular degeneration, one should include spinach, kale, Swiss chard, and other green veggies in the daily meal plan.
Regular exercise
As it is more likely for people with high blood pressure, high cholesterol, or unhealthy body mass to develop macular degeneration, regular exercise is necessary. Maintaining a healthy body mass, blood pressure, and cholesterol level can slow the condition’s progress.
Healthy lifestyle habits
People diagnosed with macular degeneration should make changes to their lifestyle. Unhealthy lifestyle habits are bad for your overall health and your eyes. Such habits expose you to dangerous toxins that can trigger cellular damage.
Wear sunglasses and hats when outdoors
If you are diagnosed with this eye condition, protect your eyes from sun exposure when outdoors. Wear sunglasses that offer good protection from UVA and UVB rays and a rating of 99 to 100 percent. Another great way to keep sunlight out of your eyes is by wearing a wide-brimmed hat. Hats stop UV rays that may escape through the top or sides of the sunglasses from entering your eyes.
Consider nutritional supplements
Taking a combination of vitamin and mineral supplements may slow the progression of macular degeneration. According to experts, consuming the supplement with a formulation that includes vitamins C and E, lutein, zeaxanthin, zinc, and copper, will benefit. It is advised to consult a nutritional expert before opting for any supplement.
Manage other medical conditions
People who have other medical conditions, such as cardiovascular disease, should make efforts to control the conditions. Taking prescribed treatments on time and following your healthcare provider’s instructions is essential in keeping macular degeneration at bay.
Only in rare instances do people go completely blind with macular degeneration. The condition can only be slowed down with the above tips and by working closely with your ophthalmologist, but it cannot be reversed.